Infusion Care in the Home
Home infusion therapy is emerging as a pivotal solution in modern healthcare, bringing IV treatments directly into patients’ living rooms.
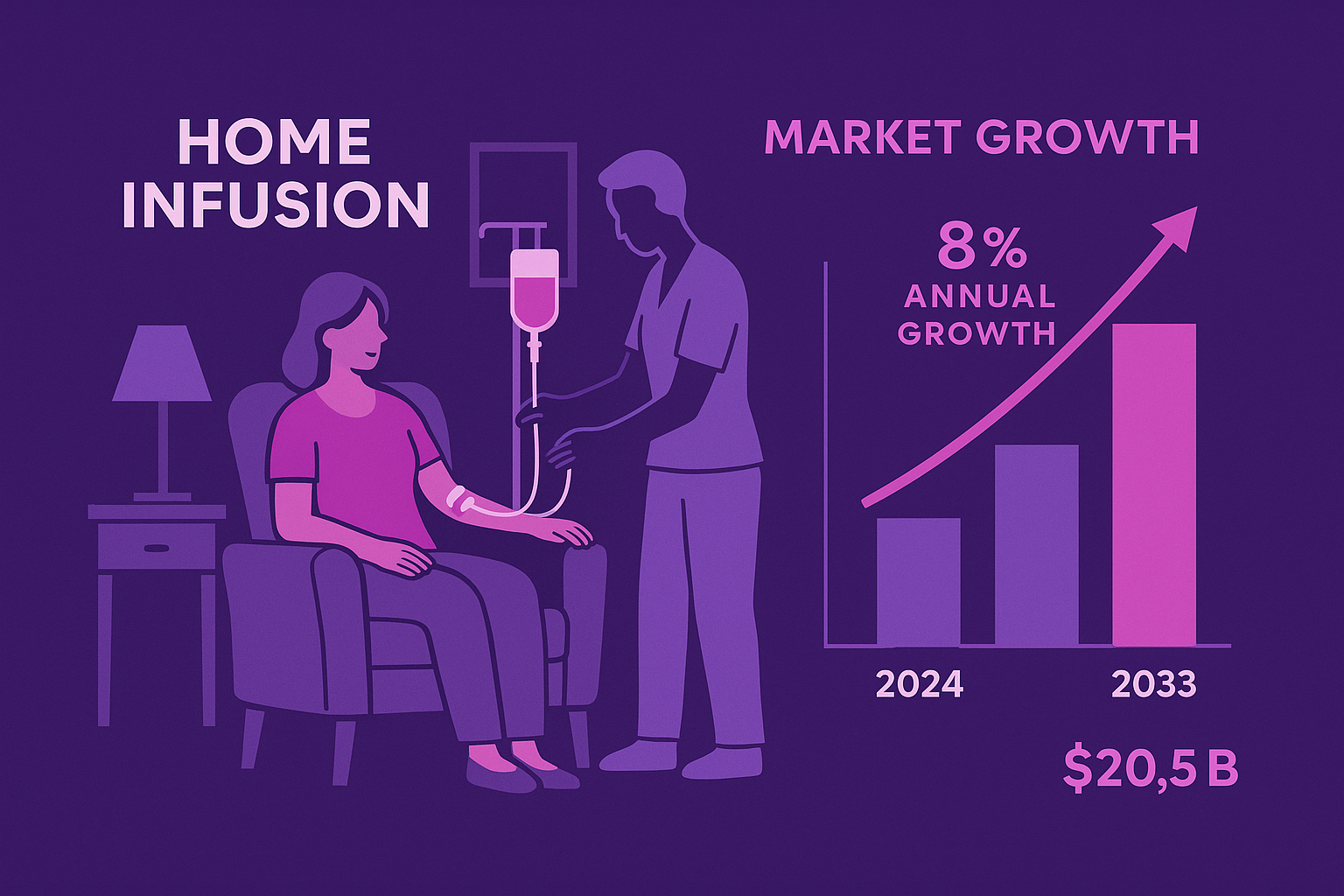
Demographic and industry trends point to surging demand: the U.S. home infusion market is projected to double from about $10 billion in 2024 to over $20.5 billion by 2033 (8% annual growth).
This growth is driven by the rise in chronic illnesses and a shift toward patient-centric, decentralized care, accelerated by the pandemic and advances in technology.
In fact, a 2022 analysis estimated that up to 25% of all Medicare services – representing $265 billion—could feasibly move from facilities to the home by 2025 without sacrificing quality.
Patients and providers alike are recognizing that many infusions traditionally done in hospitals or clinics can be delivered safely in the comfort of home, with significant benefits in convenience and quality of life.
Yet the home is a fundamentally different clinical environment, bringing both promise and pitfalls.
On the upside, receiving care at home spares patients the stress of travel and unfamiliar settings, reduces exposure to hospital-acquired infections, and lets them heal surrounded by family and daily comforts.
“Home-based infusion services are a vital component in improving access to life-sustaining IV treatments and enhancing the quality of life for patients and their families, while adding capacity to the health care system,” notes Connie Sullivan, President & CEO of the National Home Infusion Association.
On the other hand, bringing high-tech treatments into living rooms requires careful planning.
Unlike a hospital, a private home is not designed as a medical ward—safety risks, emergency preparedness, and caregiver training must all be addressed.
As Connie Sullivan observed, patients generally report they receive the same level of care at home as in a clinic, but achieving that standard demands diligent operational support.
This article explores how leading infusion programs are making safe, smart, and compassionate home-based infusions a reality.
The Safety Foundation
Preparing the Home for Infusion
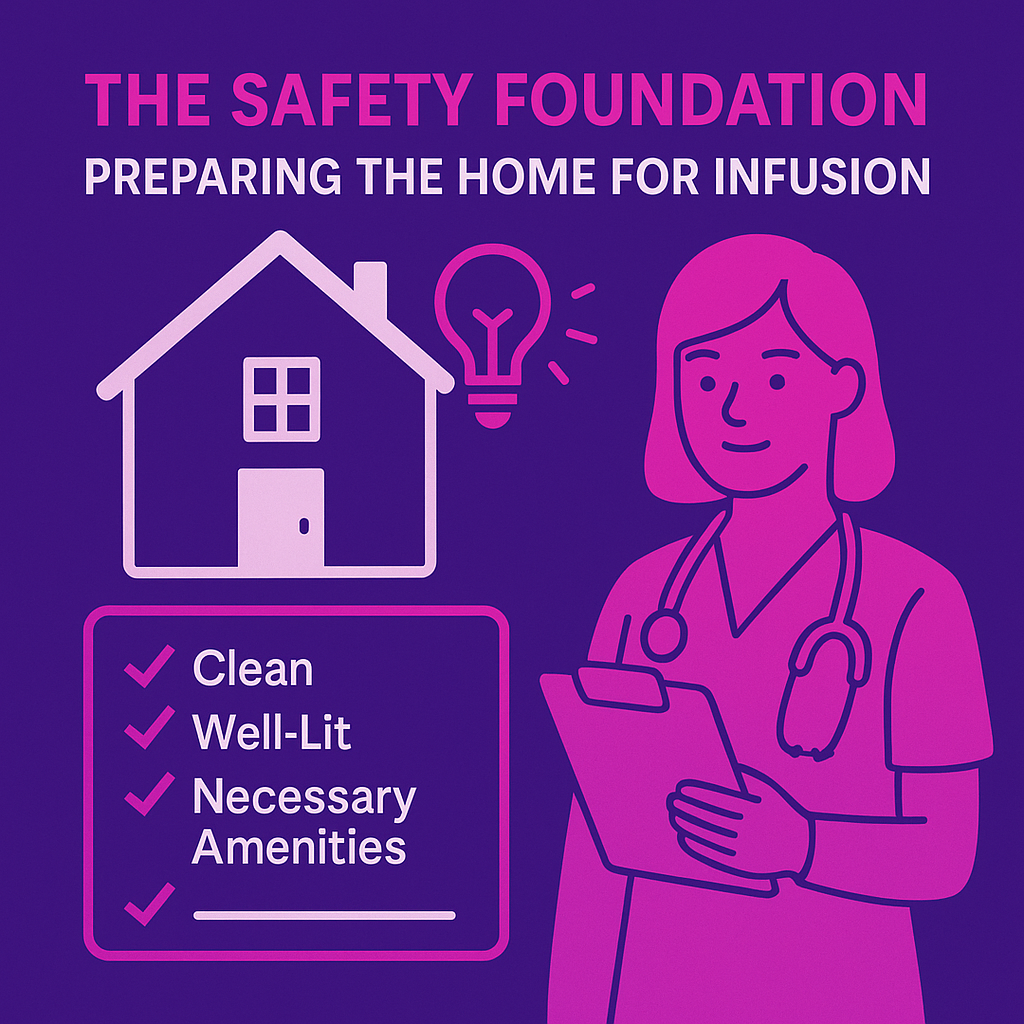
Delivering infusions at home starts with a foundation of safety.
Long before the first dose is administered, providers perform thorough pre-infusion assessments of the home environment.
A home infusion nurse or pharmacist will visit the residence to ensure it meets basic safety criteria.
Namely, the space should be clean, well-lit, and have the necessary amenities for care.
This proactive checklist helps identify any modifications needed so that the home can safely accommodate infusion therapy.
For example, the team verifies there are grounded electrical outlets and room for equipment, and that pets or environmental factors won’t compromise infection control.
Partnering with patients and caregivers is also crucial in this preparatory phase.
The best home infusion providers treat family caregivers as key members of the care team.
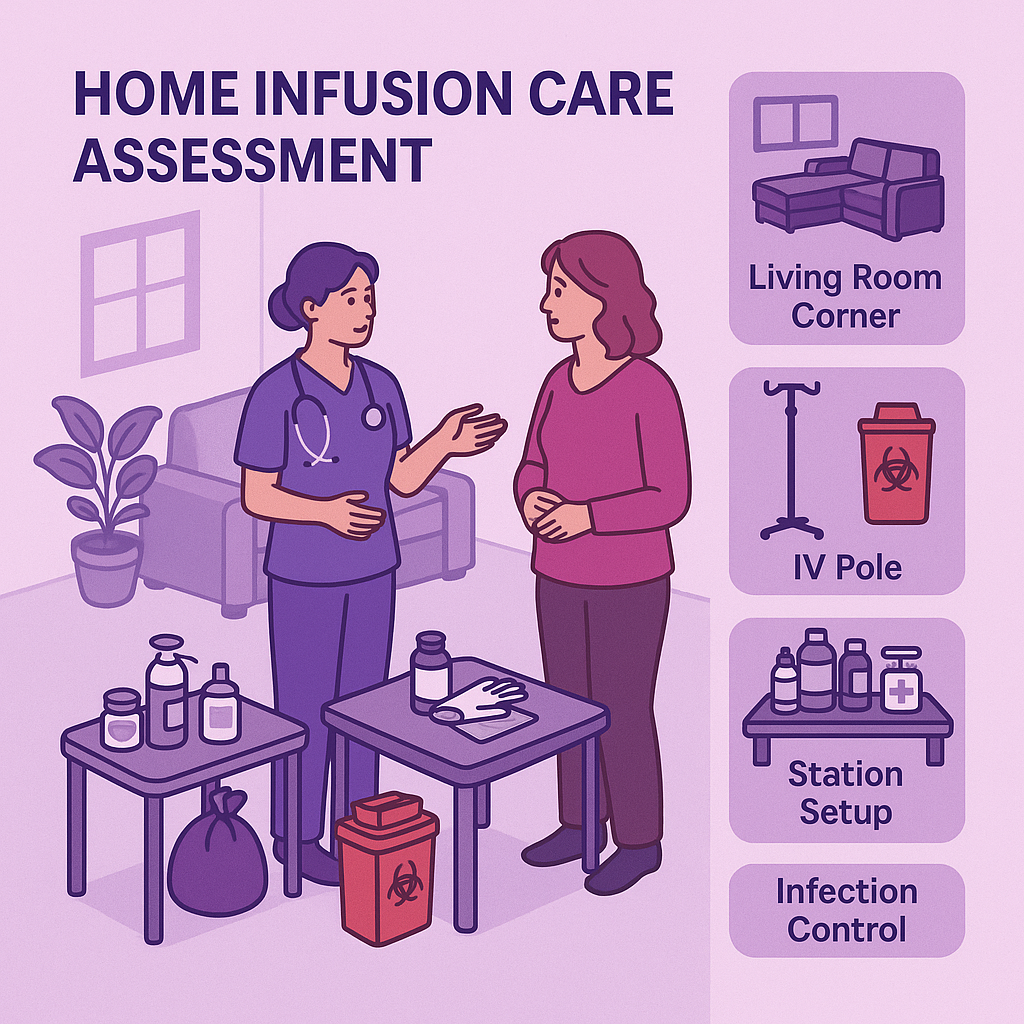
Nurses engage caregivers during the home assessment —together they decide on a suitable treatment area—often a living room or bedroom corner—discuss hygiene practices, and review the patient’s routine to minimize disruptions.
The care team may recommend simple home modifications to create a safe infusion space.
Common updates include delivering a sturdy IV pole or hook for IV bags, providing a sharps disposal container for needles, and supplying infection-control materials like hand sanitizers, gloves, and disinfectant wipes.
An initial home visit often entails setting up a small “infusion station” with a clean surface for supplies, trash bags or sharps boxes for safe disposal of used needles, and proper storage for medications.
These adjustments turn a room in the house into a safe mini-clinic for the patient’s therapy, without making it feel like a hospital.
As one home infusion nurse described, “During the initial assessment, the nurse also evaluates the patient’s home environment to ensure it is conducive to receiving infusion therapy. Factors such as cleanliness, accessibility, and proper storage of medications and supplies are taken into consideration to create a safe and comfortable treatment space.”
Technology Across Settings

Adapting Smart Tools for Home Use
One of the most exciting aspects of modern home infusion care is the way technology bridges the gap between hospital and home.
“Smart” infusion equipment and digital tools now allow complex therapies to be managed across settings with precision.
A prime example is the infusion pump itself, the programmable device that controls IV drip rates.
In hospitals, smart pumps with drug libraries and dose-error reduction software have become standard to prevent medication errors.
However, historically many home infusion providers were using simpler “dumb” pumps without these advanced safeguards.
That is rapidly changing.
Recent advances in portable infusion pumps have made it feasible to bring full smart-pump technology into the home, improving safety and accuracy for patients on IV medications.
In one study, home infusion staff were trained on ambulatory smart pumps and patients used them for a trial period.
The results showed it was a feasible and beneficial alternative to older pump models, enhancing safety without adding burden.
Today’s ambulatory infusion pumps can hold extensive medication libraries and issue alerts if a programmed dose or rate is outside safe limits—a critical safeguard in the home setting where a pharmacist isn’t on-site.
These pumps are often lightweight, battery-powered, and some even offer wireless connectivity to transmit infusion data.
Importance of Training
Training and education have also gone virtual in many cases.
During the COVID-19 era, some providers pioneered virtual infusion training for patients and caregivers, with excellent results.
For example, a hemophilia clinic used video visits to teach parents how to infuse clotting factors at home.
The virtual sessions allowed nurses to observe the family’s technique in real time and coach them through the process, greatly increasing the caregivers’ confidence.
Patients gave positive feedback, noting that the virtual “hands-on” support was a productive final step in mastering home infusion skills.
Of course, adapting hospital-grade technology to the home is not without challenges. Providers must consider digital literacy and connectivity barriers among patients.
Not every patient has reliable internet or is comfortable with apps and devices – particularly older adults or those in rural areas.
Successful home infusion programs address this by keeping tech user-friendly and offering backup options.
For instance, if a senior patient struggles with a video visit platform, the nurse can revert to a simple phone call or use specialized devices with one-touch connection.

Training is key.
Walking patients and caregivers through how to use a smart pump or a remote monitoring app is now a standard part of onboarding.
They are taught how to respond to pump alarms, how to troubleshoot basic device issues, and whom to call 24/7 for tech support.
Health agencies also step in to improve access: some provide tablets or WiFi hotspots on loan to patients who need them for telehealth.
As a recent guide on telehealth for seniors notes, common barriers like hearing or vision impairments and unfamiliarity with technology can be overcome by involving family helpers and simplifying the setup.
By acknowledging these hurdles, infusion teams ensure that “smart” care remains human-centered, not leaving anyone behind.
The thoughtful use of technology in home infusion leads to smarter, safer care.
It means a nurse can scan a patient’s infusion data remotely to double-check everything is on track, or that scheduling software optimizes nurse visit routes—innovations that translate to real operational excellence.
“To meet rising demand and benchmark quality, providers would be best-served to modernize and leverage technology that captures data accurately across all areas of operation,” advises Adrian Schauer, CEO of AlayaCare.
With the right tools in place, home-based care can be just as “smart” and connected as an infusion clinic, without sacrificing the personal touch.
Emergency Preparedness at Home

While home infusion is very safe, providers must plan for the “what if” scenarios that are normally handled by a code team in the hospital.
High-risk infusions, whether it’s a biologic that might cause anaphylaxis or a chemotherapy with potential reactions like cytokine release syndrome (CRS), require robust emergency preparedness when administered at home.
Both patients and clinicians gain peace of mind from knowing there is a “crash-response” plan in place, even if it never has to be used.
One key scenario is acute allergic reactions, such as anaphylaxis.
Infusion nurses diligently screen patients for allergy history, but unexpected anaphylaxis can occur with certain IV antibiotics, immune globulin, monoclonal antibodies, etc.
Home infusion teams therefore equip themselves with emergency medications and protocols akin to a mini crash cart.
Typically, the infusion pharmacy will dispense an anaphylaxis kit alongside the medication if a risk exists.
For example, Option Care Health (a national infusion provider) supplies kits containing epinephrine (injectable), diphenhydramine (antihistamine), a small IV saline bag, syringes, and other supplies.
Nurses servicing the home are trained in ACLS/BLS and will bring additional emergency equipment as appropriate.
Some carry portable oxygen or have an AED in their vehicle for certain cases.
The emergency protocol at home closely mirrors hospital standards: If signs of a severe reaction arise , the infusion is stopped immediately, the IV line is kept open, and 911 is called for backup.
The nurse will promptly administer epinephrine intramuscularly, then an antihistamine like diphenhydramine per the standing orders.
The patient is laid flat and monitored, with vital signs checked continuously.
The protocol might also include positioning the patient’s legs elevated if blood pressure drops. Oxygen can be given if available and the patient is struggling to breathe.
Meanwhile, emergency services are en route.
The nurse will remain with the patient until paramedics arrive, ready to initiate CPR if the rare worst-case scenario (cardiopulmonary arrest) occurs.
All these steps are clearly delineated in the care plan and reviewed beforehand so that everyone—patient, caregiver, nurse—knows their role.
In essence, the home is temporarily turned into an emergency bay until the crisis resolves or the patient is transferred to a hospital.
Thankfully, such severe events are uncommon, but this level of preparedness is what makes home infusion safe even in high-risk situations.
Consistent, Compassionate Care
The Power of One-on-One Nursing

Beyond the technology and protocols, the heart of home infusion is the one-on-one nursing care delivered to each patient.
In the home setting, patients aren’t just “another chair” in a busy infusion suite; they often develop a close therapeutic relationship with their infusion nurse.
This consistency and personal connection are powerful – fueling better outcomes, higher satisfaction, and even benefits for the nursing staff themselves.
Whenever possible, providers strive to implement consistent nurse assignments for home infusion patients.
This means the same nurse visits the patient for each infusion, rather than a rotating cast of clinicians.
Consistency allows trust and familiarity to flourish. Over repeat visits, the nurse learns the nuances of the patient’s condition, personality, and preferences – and vice versa.
Research shows that such relational continuity strongly correlates with improved patient satisfaction and confidence.
It makes sense: when patients know and trust their caregiver, they feel more comfortable voicing concerns and are more receptive to education.
One home care organization explains that regular caregivers can “develop a deeper understanding of each client’s unique preferences, needs, and routines”, leading to more proactive and personalized care.
It also spares patients the stress of repeatedly orienting new staff to their situation.
Particularly for individuals with anxiety or cognitive impairment, not having to “start over” with each visit greatly reduces confusion and stress.
In home infusion, where treatments can span weeks or months, these ongoing nurse-patient relationships become a cornerstone of compassionate care.
Patients often come to see their infusion nurse as a trusted ally, someone who is invested not just in their IV line, but in them as a person.

It’s not uncommon for patients to greet a familiar nurse with a smile and updates on their grandkids or hobbies, creating a friendly, human atmosphere around what could otherwise be a purely clinical interaction.
From the nurses’ perspective, consistent assignments can be equally rewarding.
When nurses can build lasting relationships with patients, they report greater job satisfaction and a sense of purpose in their work.
They aren’t just task-doers; they become educators, advocates, even quasi-family to the patient.
This emotional fulfillment helps buffer against burnout and compassion fatigue that are all too common in nursing.
Conversely, in settings with rotating staff, nurses might feel disconnected or constantly playing catch-up on patients’ histories.
But with continuity, a nurse can take true ownership of a patient’s care plan, see their progress over time, and gain pride in the impact they’re making.
Home care studies have noted that caregivers in consistent assignment models experience higher empowerment and fulfillment, which translates to improved retention rates.
Many infusion companies now highlight their commitment to continuity. They assign a dedicated infusion nurse to each case whenever logistics allow.
Emotional and Lifestyle Benefits of Home-Based Care
Delivering infusion therapy in the home doesn’t just keep patients physically out of the hospital; it profoundly affects their emotional well-being and daily life for the better.
Medical care that adapts to fit into someone’s life, rather than forcing life to adapt around the care, brings unique psychosocial advantages.
Home infusion, at its core, is about enabling patients to live their lives while receiving treatment, rather than putting life on hold.
One of the biggest benefits frequently reported is the ability to maintain normal routines and roles.
Patients can stick to their usual schedule as much as possible—children can attend school, working adults can continue to log in remotely or return to work sooner, and seniors can remain in their cozy home environment.
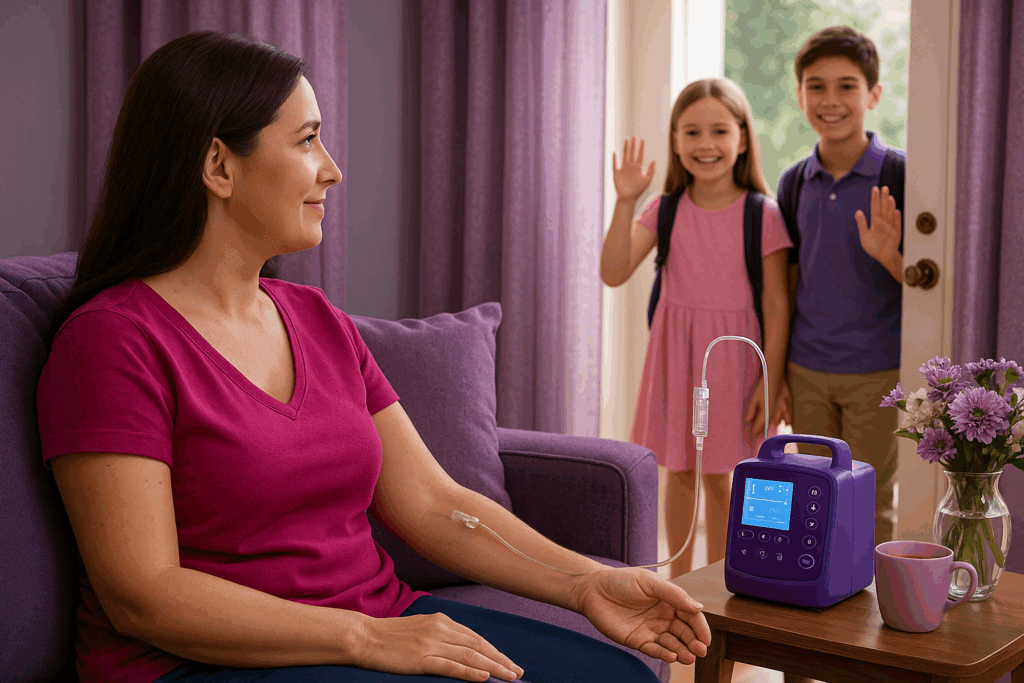
For example, a young mother on IV antibiotics can do her infusion in the early morning at home and still be there to send her kids off to school, rather than spending that time in a clinic.
Patients often say that home infusion lets them feel “normal” despite needing treatment.
They can wear their own comfy clothes, move around freely, and even sleep in their own bed during an overnight infusion.
Family involvement is another huge plus. At home, loved ones can be present and actively participate in care if the patient wishes.
Rather than sitting alone in a clinic hooked to an IV, the patient might have a spouse, parent, or friend by their side at home providing encouragement.
Family members can easily be trained by the nurse on simple tasks (like how to flush the IV line or how to disconnect the pump when it beeps).
This inclusion not only lightens the patient’s burden but also gives family caregivers a sense of contributing to their loved one’s recovery.
Comparing the Costs
Value Delivered at Home
In addition to clinical and satisfaction gains, home infusion delivers compelling economic benefits.
Comparing the costs of infusion therapy at home versus in a hospital or outpatient center reveals significant savings – for payers, health systems, and patients alike.
By avoiding the overhead of facility-based care, home infusion often provides equal treatment at a fraction of the cost, while also reducing indirect costs (like travel or missed work).
Multiple analyses over the years have confirmed the direct cost savings of home infusion.
A 2023 literature review by NHIA found consistent cost reductions across a range of infused therapies when delivered at home instead of inpatient settings.
For example, IV antibiotics are one common home therapy: one study showed the cost per day for home infusion antibiotics was about $122, versus $798 per day in the hospital.
That’s an almost 85% cost reduction, saving nearly $700 each day for each patient shifted to home care.
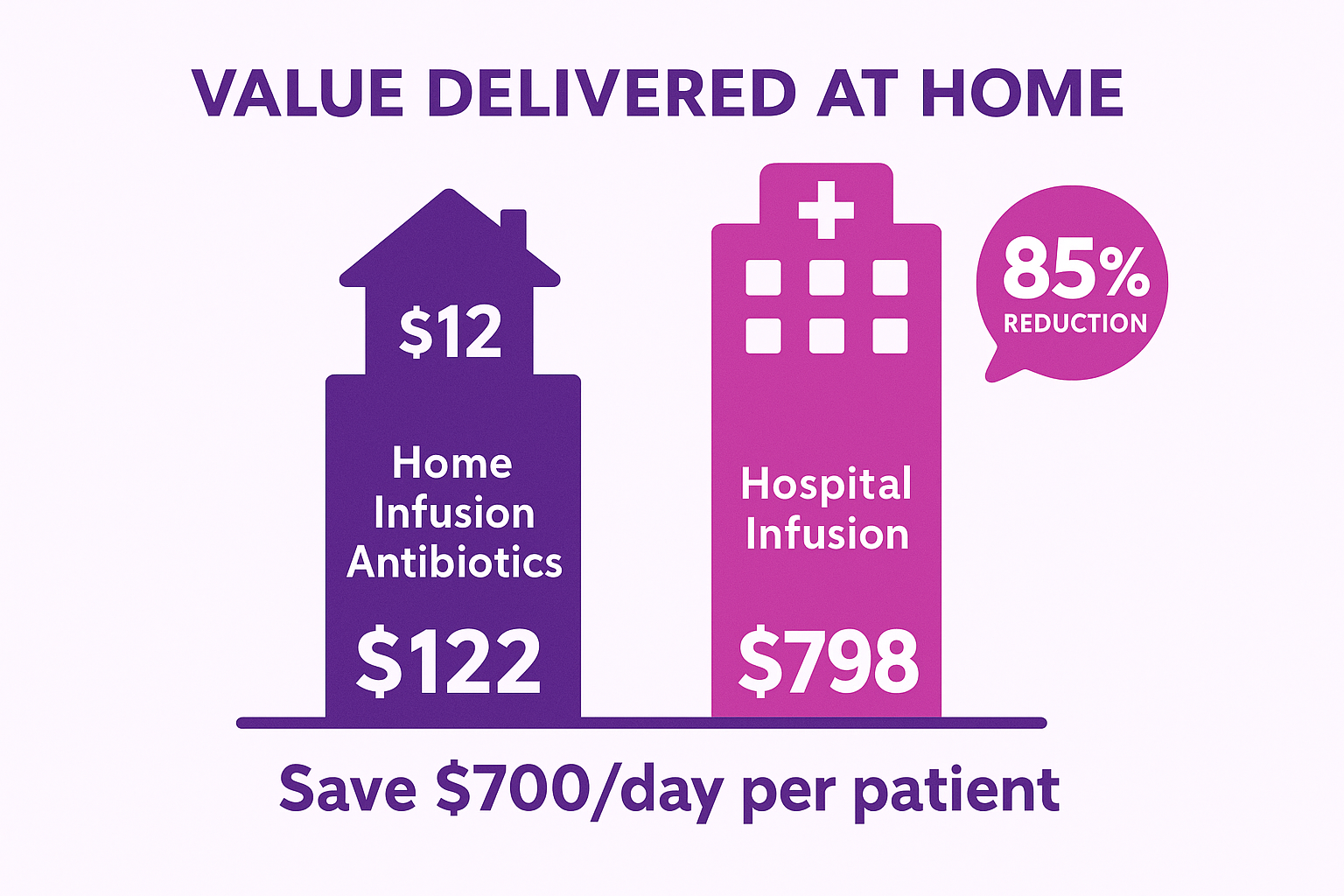
Over the course of a typical 6-week IV antibiotic course, this could mean tens of thousands saved per patient.
Another case in the literature review focused on enzyme replacement therapy and quantified the difference: average home infusion cost came out to $225 per infusion vs. $586 in hospital, about $361 less per infusion—a highly significant savings on a per-treatment basis.
High-cost chronic therapies show even more dramatic results.
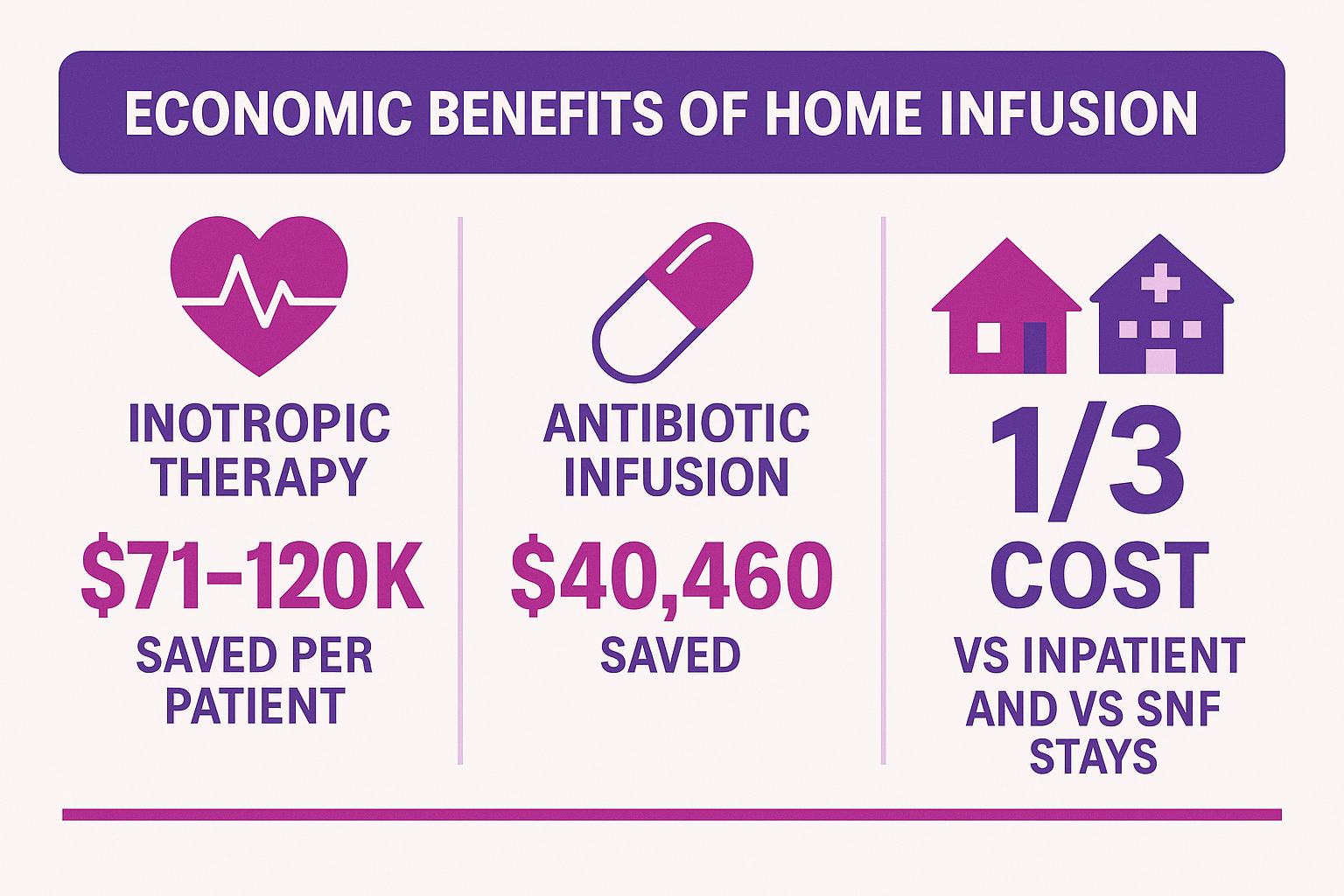
One model looking at inotropic therapy for heart failure found that treating patients at home saved $71,000 to $120,000 per patient compared to hospital care.
Another program reported an average savings of $40,460 per patient by transitioning an anti-infective (antibiotic) infusion program out of the hospital and into patients’ homes.
These figures underscore a general rule of thumb often cited in healthcare: home care can be delivered at roughly one-third the cost of equivalent inpatient care, or even less.
In fact, home and outpatient infusions are not only cheaper than hospital infusions—they are often cheaper than skilled nursing facility stays as well, making home infusion a cost-effective alternative across the board for payers.
Why are the savings so substantial? It comes down to eliminating the expensive infrastructure and overhead that hospitals carry.
When a patient receives infusion therapy in a hospital bed, charges accumulate from room fees, facility charges, ongoing monitoring, and so forth—even if the drug itself is the same.
Home infusion centralizes costs around the drug, supplies, and professional services, without paying for a bricks-and-mortar facility for each hour of care.
It’s a leaner model. The pharmacy compounds the drug and delivers it, the nurse comes to the home for a couple of hours, and that’s it.
There’s no multi-day admission or high hospital pharmacy mark-ups on the medication.
One analysis noted that hospital infusion costs can be 3 to 5 times higher than infusions delivered in non-hospital settings.
So payers (insurance companies, Medicare, etc.) have a strong incentive to encourage home infusion where appropriate, because it yields the same outcomes for far less expense.
The value proposition extends to health systems as well; by treating certain infusion patients at home, hospitals free up beds and infusion chairs for other patients who truly need acute-level care, effectively expanding capacity without new construction.
This was highlighted during COVID-19 surges when hospitals urgently needed to clear bed space; many turned to home infusion for IV antibiotics or antivirals to discharge patients sooner.
The cost savings also tie into value-based care goals: reduced hospitalization days and avoidance of complications ultimately save money in the wider healthcare continuum.
For providers and integrated delivery networks, investing in home infusion capabilities can yield a solid return on investment.
Home infusion shifts care to a lower-cost site not just in medical bills but in personal economics.
Patients can continue contributing to their jobs and caring for family, which has broad societal economic benefits.
A chronically ill parent who can get treatment at home may not need to hire a babysitter, for example, or an employee might not have to take unpaid leave.
Those are real dollars saved for households.
While harder to quantify, these factors improve the overall ROI of home-based care when looking at the big picture.
A happier, healthier patient who isn’t financially devastated by their treatment is less likely to end up using other health resources down the line—like mental health services or emergency care—further containing costs.
Home infusion therapy has proven to be a high-value proposition.
It is often safe, clinically effective, and greatly preferred by patients, while being cost-effective for payers and providers.
One publication aptly titled “Home infusion: Safe, clinically effective, patient preferred, and cost effective” concluded that home care can “improve patients’ quality of life and reduce healthcare costs”, encapsulating the quadruple aim of healthcare.
As healthcare moves toward more value-driven models, the ability to deliver safe infusion care at home positions organizations to thrive both in patient outcomes and financial sustainability.
Case studies and modeled scenarios consistently bear out that when you factor in direct medical costs and indirect benefits, home infusion delivers outstanding value.
It is value delivered at home, in every sense of the phrase.
Summary
A Framework for Expanding Safe Home Infusion Services
Home infusion is no longer a niche alternative.
It’s fast becoming a mainstream component of care delivery.
To successfully expand these services while safeguarding quality, providers must adopt a comprehensive framework of operational best practices, safety protocols, and supportive systems.
As we’ve explored, the pillars of such a framework include.
Meticulous home preparation and safety checks, integration of smart technology and telehealth across settings, rigorous emergency planning, continuity in staffing, compassionate patient-centered culture, and a keen eye on cost-effectiveness.
By investing in strong support systems.
Scheduling logistics, supply chain coordination, electronic documentation, and regulatory compliance organizations ensure that the home infusion program runs smoothly behind the scenes.
For instance, efficient scheduling and routing of infusion nurses is vital to cover widely distributed patients.
Robust documentation is essential for tracking each patient’s treatments, inventory of meds/supplies, and meeting accreditor requirements.
Ongoing staff training and competency validation keep the team ready to handle new therapies and maintain readiness for audits or emergencies.
Quality assurance mechanisms, like patient satisfaction surveys and outcome tracking, help continuously improve the service.
In short, success in home infusion hinges not on any single factor, but on a well-orchestrated system that blends clinical excellence with operational rigor.
Healthcare organizations looking to develop or scale a home infusion program don’t have to do it alone.
With deep expertise in infusion management services, our team at Infusion Management HQ supports clients in building high-quality home infusion capabilities.
Helping you foster a patient-focused culture, develop nurse assignment models that promote consistency, and implement patient education frameworks that empower caregivers.
As demand for home infusion continues to grow, having a robust operational framework in place will position your organization to expand services confidently and quickly, without compromising on care.
The future of infusion therapy is unfolding at home—delivering IV medications with a personal touch, aided by technology and guided by proven practices.
Providers that embrace this shift will improve patient satisfaction and outcomes, all while controlling costs and extending their reach.
If you’re ready to take the next step in elevating your infusion services, we invite you to continue the journey with us.
Download our “Home Infusion Implementation Guide” to get a detailed blueprint for establishing and scaling a successful home infusion program.
This free guide is packed with checklists, policy templates, and real-world case studies to help you deliver safe, human-centered infusion care at home—and reap the rewards for your patients and organization alike.
Let’s bring infusion therapy home together.



